When is it indicated?
Women without ovarian function
Premature ovarian failure:
These are considered to be situations in which menopause occurs at an age below 40 years.
The causes are very different, including genetic factors, surgical and oncological treatments (chemotherapy and radiotherapy).
Primary ovarian failure:
This includes situations due to genetic and developmental defects that do not allow menstruation to occur from puberty (Pure gonadal dysgenesis: 46XX, Turner syndrome: 45XO, Swyer syndrome: 45XY, Savage syndrome).

Women at higher risk
- Women who are carriers of some type of hereditary disease that cannot be performed by Preimplantation Genetic Diagnosis.
- Women with ovaries that are inaccessible for the collection of oocytes.
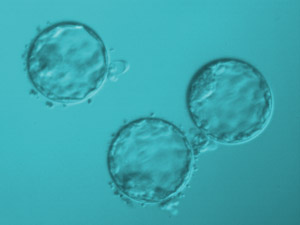
- When repeated attempts at In Vitro Fertilization have not been previously successful (poor oocyte quality, low response and implantation failure).
- Women with a history of repeated miscarriages.
- Women over 40 years of age who, despite having ovarian function, are of an advanced age that does not allow them to obtain a good number of good quality oocytes or even an increased risk of Down Syndrome.